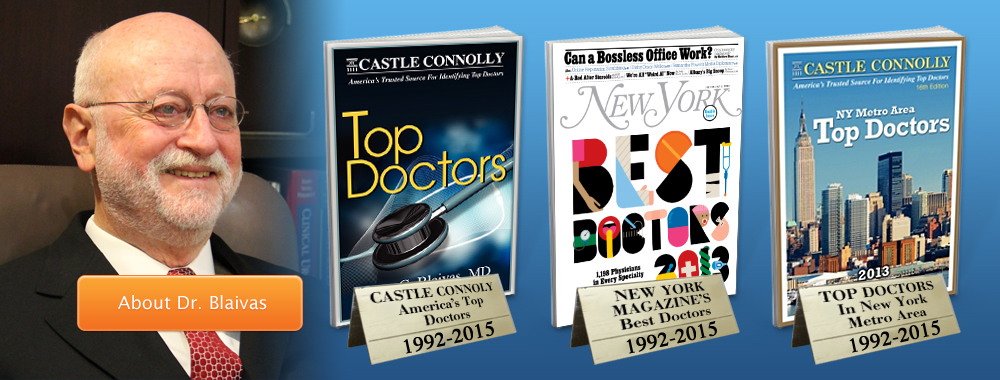
Jerry G. Blaivas, MD, FACS Dr. Blaivas is a world-renowned urological expert, surgeon, distinguished author, educator, and medical pioneer. He was one of the founders of urodynamics and established many of the current surgical procedures used to correct stress incontinence, urinary fistulas, urethral diverticulum, overactive bladder and neurogenic bladder. He is also one of the… Continue Reading
See Our Main Site www.UroCenterofNewYork.com Blog Posts are Below: Continue Reading
Category Archives: Urology
Why do urethral strictures recur after a urethral dilation or urethrotomy?
by Rajveer S. Purohit, MD, MPH
A urethral stricture is a narrowing of the urethra caused by scar tissue but we often refer to the condition with the phrase urethral stricture disease. Sounds similar but a key difference is that last word “disease” and that goes a long way to explaining some of the critical ideas to understanding the nature of the problem. Urethral stricture disease refers not only to the narrowing of the lining of the urinary tube (the urethra) by scar tissue but refers to scar tissue that underlies the channel. To understand this better, imagine the urethral as a long tubular donut with the hole (the lumen) being where the urine is carried. The spongy part of the donut is called the corpus spongiosum (spongy body) and is a rich vascular network that carries oxygen and nutrients to the inner lining of the hole (the urethra) to keep it healthy.
 Urethral stricture disease, then, refers not only to scar tissue that closes the urethra, or a urethral stricture, but also refers to the presence of scar tissue in the corpus spongiosum, in a process called spongiofibrosis. Spongiofibrosis prevents vital nutrients and oxygen from getting to the urethra and keeping it healthy. Urethral stricture disease than is a urethral stricture with underlying spongiofibrosis.
Urethral stricture disease, then, refers not only to scar tissue that closes the urethra, or a urethral stricture, but also refers to the presence of scar tissue in the corpus spongiosum, in a process called spongiofibrosis. Spongiofibrosis prevents vital nutrients and oxygen from getting to the urethra and keeping it healthy. Urethral stricture disease than is a urethral stricture with underlying spongiofibrosis.
It is clear from this description why the failure rate for urethral dilation or urethrotomy (endoscopic incision into the urethral stricture) is high, particularly for those patients with dense, long strictures and extensive spongiofibrosis. If the donut hole is forcibly opened with a dilator or cut the underlying scar tissue, or spongiofibrosis, is still not corrected. Over time the absence of a healthy blood supply to the lining causes the stricture to recur. In fact, there is increasing data to suggest that every time you do a dilation or urethrotomy to open a stricture you can also cut into the delicate corpus spongiosum and cause further scar tissue or spongiofibrosis to form. This in turn makes recurrences after dilations more dense and often longer than the original.
Although there is a high failure rate after a urethral dilation, there is a role for it in some circumstances as we’ll discuss in a future blog post.
Urology
Urology (from Greek οὖρον ouron “urine” and -λογία -logia “study of”), also known as genitourinary surgery, is the branch of medicine that focuses on the surgical and medical diseases of the male and female urinary tract system and the male reproductive organs. The organs under the domain of urology include the kidneys, adrenal glands, ureters, urinary bladder, urethra, and the male reproductive organs (testes, epididymis, vas deferens, seminal vesicles, prostate and penis).
The urinary and reproductive tracts are closely linked, and disorders of one often affect the other. Thus a major spectrum of the conditions managed in urology exists under the domain of genitourinary disorders. Urology combines the management of medical (i.e., non-surgical) conditions such as urinary tract infections and benign prostatic hyperplasia, with the management of surgical conditions such as bladder or prostate cancer, kidney stones, congenital abnormalities, traumatic injury, and stress incontinence.
Urology has traditionally been on the cutting-edge of surgical technology in the field of medicine; including minimally invasive robotic and laparoscopic surgery, laser assisted surgeries, and a host of other unique scope-guided-procedures. Urologists are well-trained in open and minimally-invasive techniques, employing real-time ultrasound guidance, fiber-optic endoscopic equipment, and various lasers in the treatment of multiple benign and malignant conditions.[1] In addition, urologists are pioneers in the use of robotics in laparoscopic surgery. Urology is closely related to (and urologists often collaborate with the practitioners of) the medical fields of oncology, nephrology, gynaecology, andrology, pediatric surgery, colorectal surgery, gastroenterology, and endocrinology.
Urology is one of the most competitive and a highly sought-after surgical specialty to enter for physicians, with new urologists comprising less than 1.5% of U.S. medical school graduates each year.[2][3] In Canada, Urology is an exceedingly difficult specialty to match, with less than 0.1% of the position dedicated to Urology.
Urologic surgeons, or urologists, undergo a very rigorous post-graduate surgical training period for a minimum duration of five years, of which 12 months must be completed in general surgery and 36 months must be completed in clinical urology. The remaining 12 months are spent in general surgery, urology or other clinical disciplines relevant to urology.[4] Upon successful completion of a residency program, many urologists choose to undergo further advanced training in a sub-specialty area of expertise through a fellowship lasting an additional 12 to 36 months. These may include: urologic surgery, urologic oncology and urologic oncological surgery, endourology and endourologic surgery, urogynecology and urogynecologic surgery, reconstructive urologic surgery (a form of reconstructive surgery), minimally-invasive urologic surgery, pediatric urology and pediatric urologic surgery (including adolescent urology, the treatment of premature or delayed puberty, and the treatment of congenital urological syndromes, malformations, and deformations), transplant urology (the field of transplant medicine and surgery concerned with transplantation of organs such as the kidneys, bladder tissue, ureters, and, recently penises), voiding dysfunction, neurourology, and androurology and sexual medicine. Additionally, some urologists supplement their fellowships with an additional Masters (2-3 years) or a PhD (4-6 years) in related topics to prepare them for an academic as well as a focused clinical job.
Urologic Problems in Men BPH and other urinary issues Incontinence Kidney Stones Sexuality & Hormones Prostatitis Prostate cancer treatment complications Urethral stricture Urological cancers Continue Reading
Urologic Problems in Women Incontinence Mesh Complications Vesico-vaginal fistula Prolapse (dropped bladder) Nocturia Urological cancers Urinary infections Kidney stones Neurogenic bladder Continue Reading